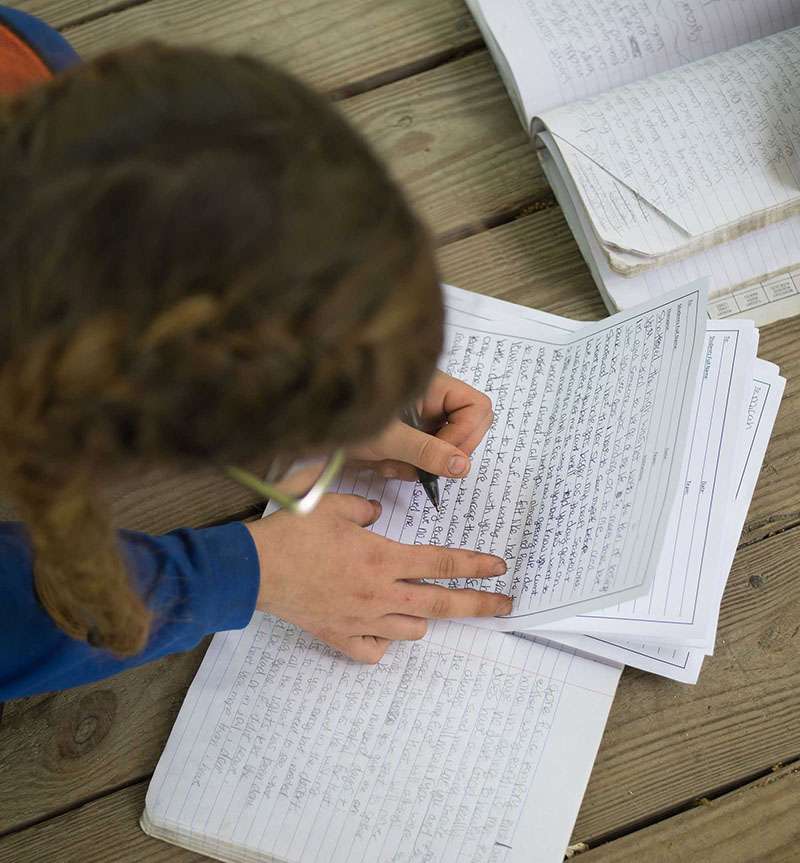
Adventure Wilderness Program for Students 10-17
At Trails Carolina, our wilderness therapy program’s mission is to give your child the confidence, coping mechanisms, and communication skills that will help them become the best version of themselves. Throughout our wilderness program, families restore and rebuild their relationship with their child.
We believe that by connecting with nature in a wilderness therapy setting, your child can learn to address their unhealthy behaviors, gain valuable personal insights, and learn important lessons. Free from the distractions and negative influences of everyday life, they can focus on their own personal growth and healing process.
Our multidisciplinary team of caring, expert staff will be there to guide your child along their unique path to psychological and emotional wellness. This journey can lead to a renewed sense of self and a happier, healthier future brimming with opportunity.
Building Resilience Through Residential Therapy
Our programming is designed around transitions and healing the entire family. We want your child to practice their newfound skills in a variety of challenging environments, building resilience that will allow them to easily carry these positive behaviors into the real world. At the same time, it’s important that you as a parent are empowered with new approaches to support your child’s success.
Wilderness Therapy
We believe that a wilderness setting combined with a residential treatment center enhances the benefits of therapy.

Lasting Change
We believe that practicing and applying the lessons learned in the wilderness to everyday situations promotes lasting change.
Family Involvement
We believe that families benefit from being involved in their child's process.
Get started today
Contact us today to learn how Trails Carolina can help your family
Trails saved my daughter’s life. Amanda is an amazing human and a brilliant therapist. I am so grateful to her, Science Steve, and the other wonderful people who could reach my daughter at a time when I could not.
Margot Lowman August 2022
Great life changing experience for our son. After becoming addicted to gaming during covid he was very depressed. At Trails he experienced the wilderness, Science Steve, learning survival skills and top notch therapy and support etc… I highly recommend! This gave our son and our family a renewed family bond full of love and excitement about his bright future.
Winnifred Wilson July 2022
Outstanding clinical work and superb staff! There’s a great culture at this company and it shows with how they engage with families/clients.
Kristin Brace June 2022